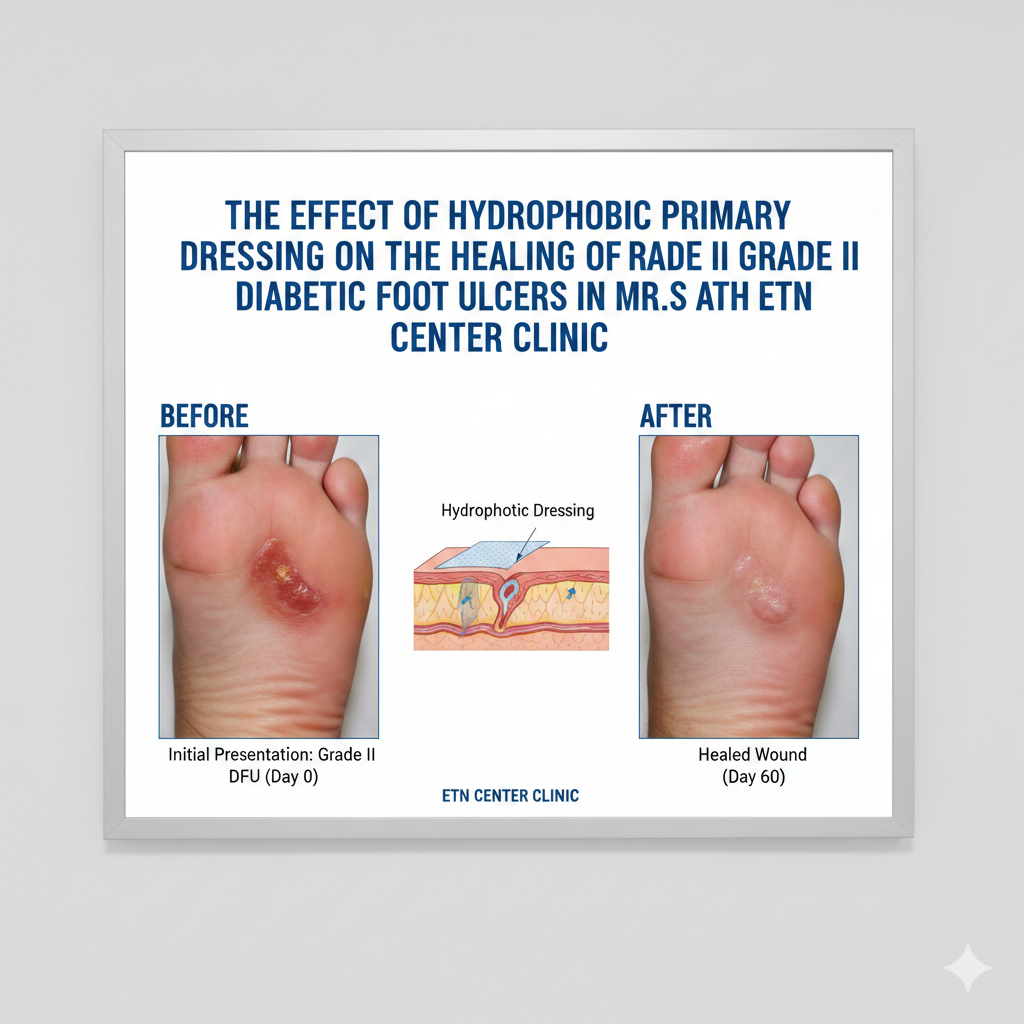
The Effect of Hydrophobic Primary Dressing on the Healing of Grade II Diabetic Foot Ulcers in Mr. S at the ETN Center Clinic
Keywords:
Nursing care, Hydrophobic, Diabetic foot ulcerAbstract
Background: Diabetic foot ulcers are serious complications in patients with diabetes mellitus that often exhibit delayed healing due to vascular impairment, neuropathy, and a high risk of infection. The use of modern wound dressings such as hydrophobic dressings offers an innovative approach through a physical mechanism that binds microorganisms without inducing antimicrobial resistance, thereby potentially accelerating the wound-healing process. Objective: To identify the effect of hydrophobic dressing as a primary dressing on the healing of grade II diabetic foot ulcers through a comprehensive nursing care approach. Methods: The study used a case study design by implementing a complete nursing care process that includes wound assessment, nursing diagnosis determination, intervention planning, action implementation, and evaluation of treatment outcomes. Wound observations were conducted serially at three time points (July 21, August 15, and August 20, 2025) using the Bates-Jensen Wound Assessment Tool (BJWAT). Treatment procedures included wound cleansing with antiseptic soap, application of PHMB to reduce the microbial load, application of a hydrophobic dressing as a primary dressing, and use of a secondary dressing to maintain optimal wound moisture. Evaluation included measurement of wound size, percentage of granulation tissue, slough, epithelialization, exudate characteristics, and patient pain response. An educational approach was provided to support patient compliance with foot care and blood sugar control.. Results: Wound healing showed significant improvement during treatment with hydrophobic: On July 21, 2025, the wound tissue consisted of 40% slough, 60% granulation, and <25% epithelialization, with a wound area of 2.5 cm². On August 15, 2025, granulation increased to 90%, slough decreased to approximately 10%, and epithelialization increased to 25–<50%, with a wound size of 1 cm². On August 20, 2025, granulation reached 100%, slough 0%, epithelialization 25–<50%, and the wound size decreased to 0.08 cm². Acute pain initially reported as a scale 2 resolved within one intervention session. Conclusion: The use of hydrophobic dressing as a primary dressing in nursing care proved effective in accelerating the healing of grade II diabetic foot ulcers by improving the wound condition objectively and reducing the patient’s subjective complaints.